In this blog, we want to elaborate on ventilation and COVID-19. An essential approach to reducing the concentrations of inside air pollutants or contaminants containing each virus that might be in the air is improving ventilation – the amount of outdoor air coming inside.
Ensuring adequate ventilation with outside air can help lower the concentration of airborne contaminants, including viruses indoors. However, by itself, improving ventilation is not enough to protect people from COVID-19. When used along with other best practices advised by the Centers for Disease Control and Prevention (CDC) and others, improving ventilation can be a plan to protect people in close areas. And this is where the impact of ventilation and COVID-19 illuminates.
Generally speaking, when the number of people in an indoor environment increases, ventilation with outdoor air arises more. The ventilation rate should be regarding the number of individuals living in an indoor space and some other factors. Simply put, indoor spaces can be more dangerous than outdoor areas since it might be harder to keep people apart, and there’s less fresh air. Give special attention to increased ventilation when occupancy is high.
Also, make sure that high-traffic regions have additional ventilation. In addition to reducing the risk of the airborne transmission of viruses, improving ventilation also improves indoor air quality and limits exposure to materials used to clean and disinfect contaminated surfaces.
Homes, Ventilation, and COVID-19
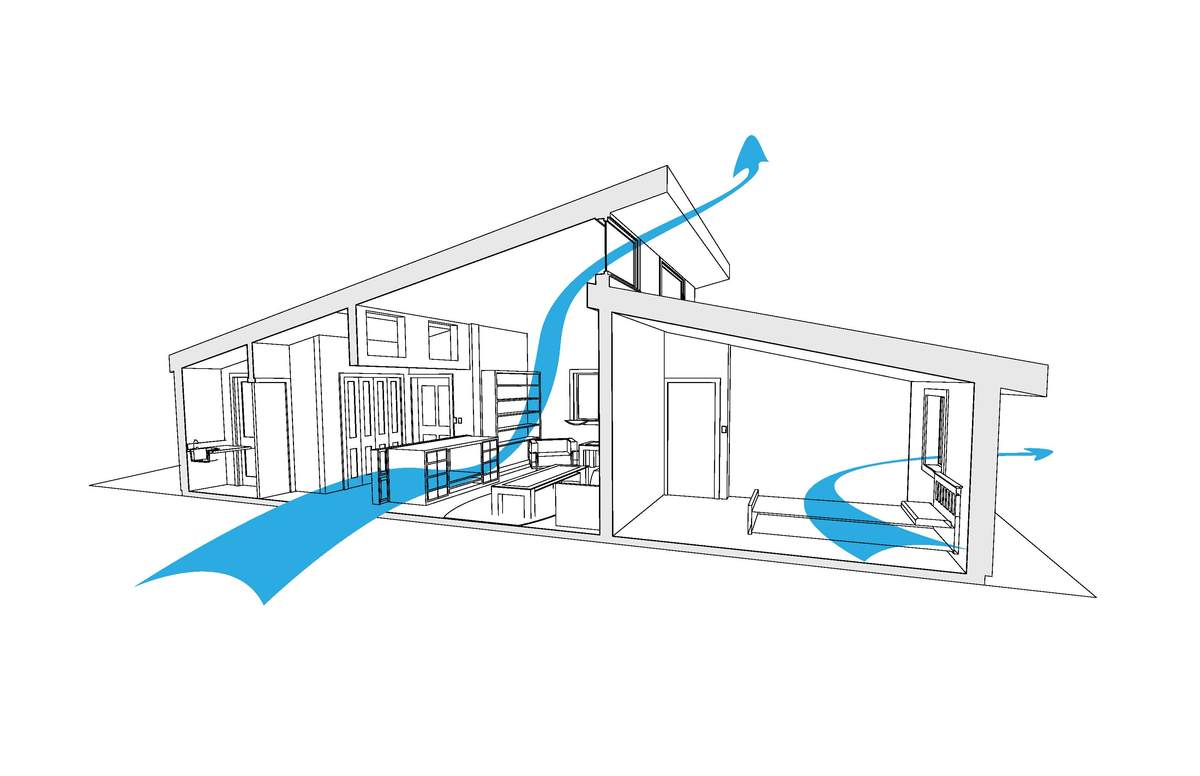
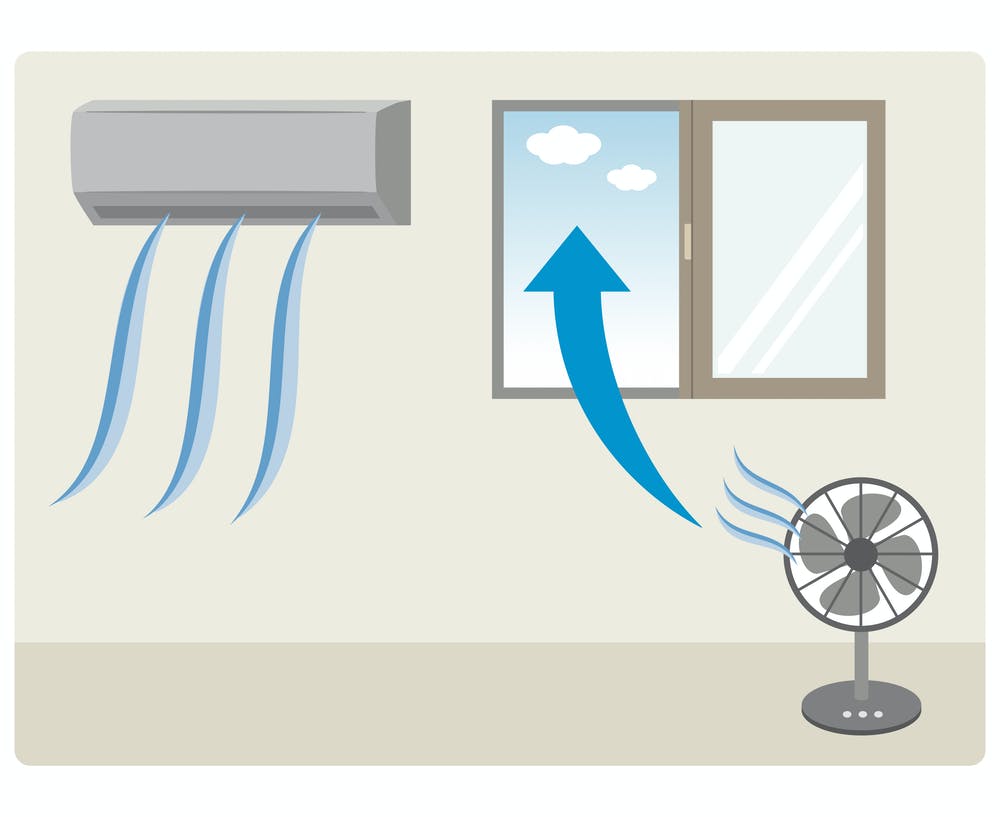
Opening windows and doors in moderate weather conditions, using window or attic fans, or running a window air conditioner with the vent control speeds up the home’s outdoor ventilation rate. Do not open windows and doors if it poses a safety or health risk to children or other family members (e.g., risk of falling or triggering asthma symptoms). Local bathroom or kitchen fans exhaust outdoor air and remove contaminants directly from the room where the fan is located increasing the air outdoors’ ventilation rate.
Ventilation and COVID-19 in Offices, Schools, and Commercial Buildings
Most offices, schools, and commercial buildings have heating, ventilation, and air conditioning (HVAC) systems with filters on them. Typically, building or HVAC specialists maintain these systems. Professionals who operate the mentioned buildings should use the guidance of ASHRAE (American Society of Heating, Refrigerating, and Air-Conditioning Engineers) and other experts and government organizations for information about ventilation and air filtration to help to reduce the risks from the virus causing COVID-19.
In general, improving ventilation and filtration is often proper; but, due to the diversity and complexity of building sizes, types, construction styles, HVAC system components, and other building features, a professional should adhere to ASHRAE guidelines for their specific building and circumstances.
In the concept of ventilation and COVID-19, improving ventilation with all or mostly outside air may not always be possible or practical. In these cases, the effective ventilation rate per person can also be increased by controlling the number of occupants present in the building in general or in specific rooms.
Administrative practices encouraging remote participation and reducing room occupancy can lower the risks of COVID-19. ASHRAE consultancy helps gain information about ventilation rates for different types of buildings and other essential engineering actions to control ventilation, moisture, and temperature in a building. To find more information about what ASHRAE said about Ventilation and COVID-19, click here.
Ventilation and COVID-19, cleaning and disinfection
Ventilation is necessary when cleaning and disinfecting for COVID-19. According to their label instructions, using EPA-registered cleaning and disinfecting goods is the best way to ensure that any indoor air pollution dangers are reduced while still maintaining the disinfecting product’s effectiveness. In particular, follow any label precautions that suggest wearing personal protective equipment, like gloves or eye protection, designed to protect those who use the product. As a general forethought, do not mix cleaning or disinfecting products.
Generally, improving ventilation during and after cleaning, such as opening windows or doors, limits exposure to cleaning and disinfection products and byproducts. Improving ventilation can also lower risks from particles suspended during cleaning, including those potentially carrying SARS-CoV-2 (or other contaminants).
If possible, sensitive individuals should avoid cleaning and consider leaving the room during the auction. Sensitive individuals may include pregnant women and people with asthma disease. Also, sensitive people should not be present when disinfectants are being used. You should store and use chemicals out of the reach of children and pets. Avoid ventilation with outdoor air when it is polluted or makes your home too cold, hot, or humid.
Do HVAC systems directly have a role in COVID-19 transmission?
Up to this time, there is no evidence of COVID-19 transmitting through the ductwork of an HVAC system to infect individuals in other rooms or other areas in a building. In cases where ventilation has played a role in outbreaks, the ventilation failure affected individuals in the same room and precisely at the same time as the index patient is there.
This contrasts with other airborne diseases such as chickenpox or measles, which can travel meters or transmit to others even after the index case has left the supposed site of infection (for example, the pediatric waiting room). Being close to the index case appears to have a severe role in COVID-19 transmission.
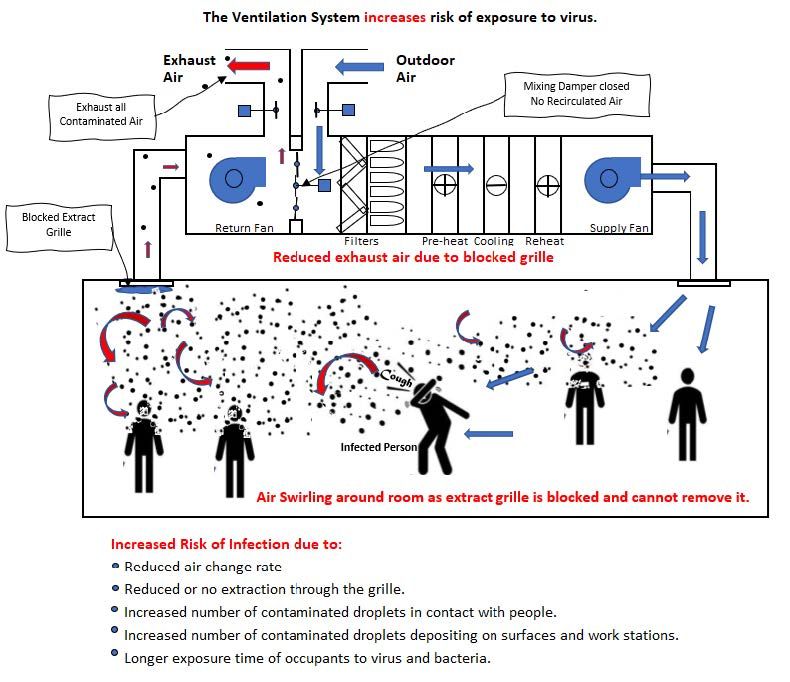
Possibly the most closely examined (and most publicized) example of possible short-range aerosol transmission happened in a restaurant in the early days of the pandemic. At first, transmission from the index patient to nine other people happened because of a small split air conditioner pushing large droplets farther than anticipated. However, additional studies using tracer gas measurements and airflow simulations unveiled that the room also had minimum fresh air input (<1 L/s per person), and also the exhaust grilles were sealed.
The only ventilation was provided by people who regularly opened the fire door. This lack of airflow, in addition to local air conditioning, might have formed a small pocket of air at one location of the room in which droplets from the index patient could have accumulated and circulated, which resulted in short-range aerosol transmission to those who also spent enough time in the pocket (more than 4 m away). No staff or patrons outside that district were infected, which might have resulted from this pocket influence or the dilution of particles as they diffused away from the source.
Thus, spaces with insufficient fresh air supply and/or unbalanced supply and return airflows may create the opportunity for COVID-19 particles to build up and transmit more efficiently past 2 m. Therefore, HVAC systems’ most likely role in the pandemic is alleviating close-range transmission between people sharing the same space rather than spreading the disease to distant locations.
Another sample in which we might wait to see advanced disease transmission is when turbulent or profoundly directional airflow either hinders particles from settling or directly conducts particles from one person’s breathing area into another’s. An example of this concept may have occurred during a bus trip, in which the index patient spread the virus to 22 other passengers dispersed throughout the bus. Remarkably, passengers sitting near the only open window did not contract the virus. The authors attributed the diffusion throughout the bus to recirculation through the air conditioning system; however, dispersion could also have been achieved by the strong drafts from the open window.
As a result of these incidents, a great deal of concern has been raised regarding employing fans and air conditioners. Guidance documents regularly recommend against blowing air across several people but rather direct the airflow upward or at a wall to cool the location without creating drafts. In addition, because fans and air conditioners recirculate the air in the room without filtration, they should only be used in rooms with satisfactory ventilation. It should also be mentioned that extreme heat can be dangerous. In communities where the COVID-19 case rates are low, the risk of death resulting from heat intensity may be higher than that of COVID-19. In such cases, air conditioners and fans may be life-saving devices, which can and should be used with the precautions aforementioned above.
Fewer faces resulted from bigger spaces
In the concept of ventilation and COVID-19, several other incidents have been largely or uncritically attributed to insufficient ventilation, such as an outbreak in a Zumba fitness class or call center. This assumes that sufficient or even improved ventilation could have inhibited or restricted the outbreak.
In the case of the Zumba class, participants were involved in high-intensity activities which generated lots of droplets for 50 minutes. On the other hand, the participants danced back and forth through the turbulent plumes of droplets produced by their classmates’ inhalation and exhalation. Moreover, in the case of the call center, outbreaks included crowding, constant vocalization (talking, warbling), and regular mixing/interaction.
Since all of these events presented an adequate opportunity for exposure to those larger and higher-risk droplets, it is unclear whether improved ventilation would have had a notable effect on minimizing transmission. This does not mean that ventilation cannot effectively diminish droplet numbers. Some researchers recently demonstrated that opening a window in a well-ventilated room lowered the half-life of 5 micrometers droplets to 30 sec compared to about 5 min in an unventilated apartment. However, the most practical means of reducing transmission when bodies congregate is to lessen the production of droplets (source control or more scattered people) and restrict the overlap of breathing zones (use of partitions and controlled crowding).
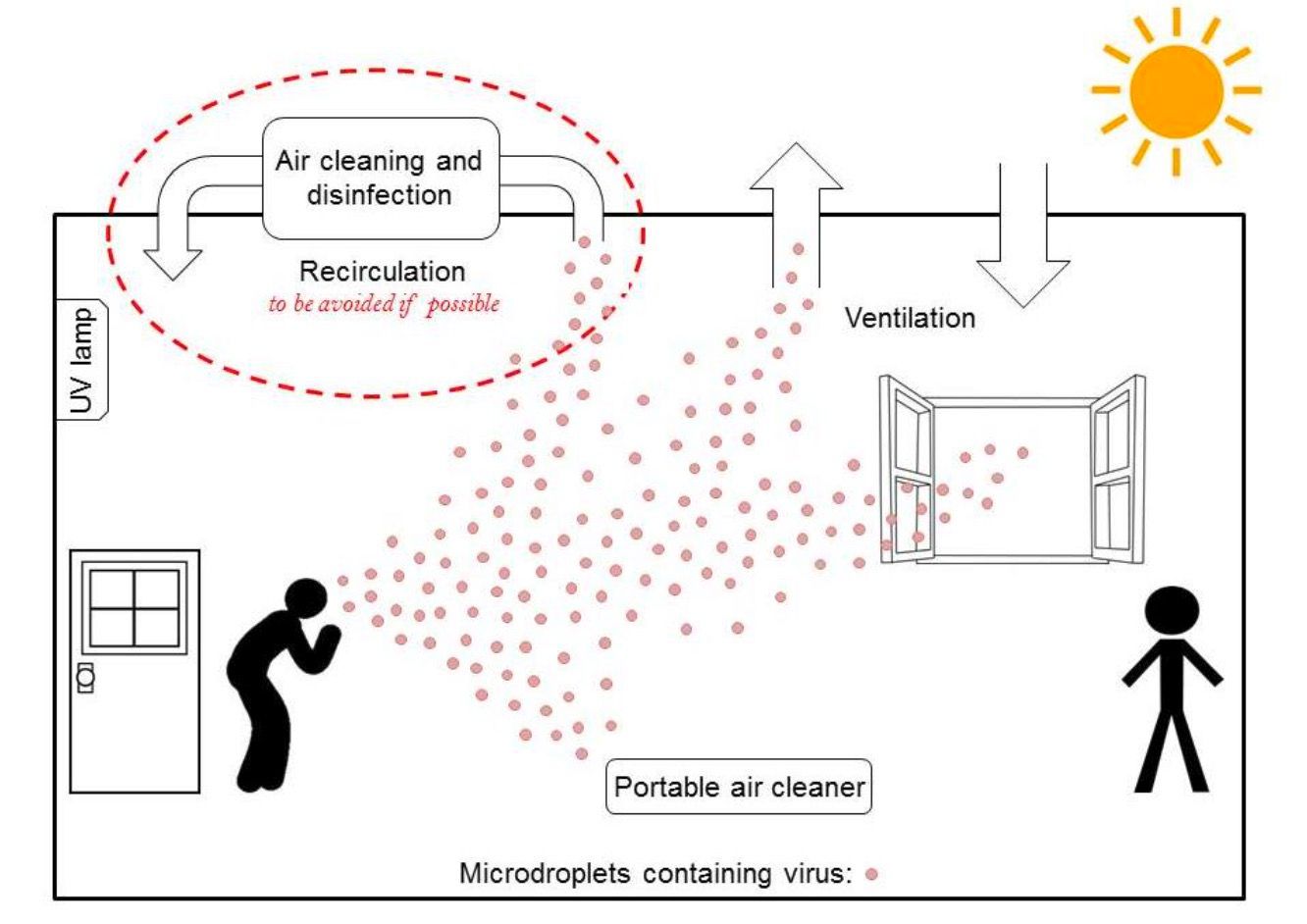
In ventilation and COVID-19, given the risks of under-ventilated spaces, duct air filters, and portable air cleaners came interested as a tool for lowering COVID-19 transmission. Although there is no clinical evidence to show that air filtration affects COVID-19 transmission, properly operating units with firmly sealed filters should reduce respiratory particles in the air, which may reduce the likelihood of transmission. However, as emphasized above, these devices should not be relied upon as a primary means of infection control, as poor placement or home maintenance of the device may render them less effective or create a false sense of security. The first and most important means of reducing transmission in any space is to diminish crowding.
Three easy-going ways to have proper ventilation and COVID-19
World Health Organization (WHO) has established guidance on Ventilation and COVID-19, which can be found here. WHO works jointly with the World Meteorological Organization Joint Office for Climate and Health. It also collaborates with the United States National Oceanic and Atmospheric Administration (NOAA) through the Global Heat Health Information Network to establish and update this guidance.
Data collected and released by the WHO about Ventilation and COVID-19 indicates that poor ventilation brings about virus transmission enhancement. Therefore, improving indoor ventilation should be considered a crucial step in reducing the spread of viruses such as COVID-19. Here we have provided three simple steps to make indoor ventilation better and minimize the risk of COVID-19 transmission in order to meet the ventilation and COVID-19 do’s and don’ts.
1. Open Windows and Doors
Opening a window or a door is a simple method to develop ventilation indoors. Data reveals that opening windows in a typical home can double ventilation rates. Moreover, scientists found that opening windows in old-fashioned hospitals with large windows and high ceilings increased air change almost 20 times.
Scientists in the US also tested how ventilation rates varied when opening the frontal door of a regular home. They also found that opening the door 60 times in an hour duplicated the ventilation rate.
Opening a window or door is an uncomplicated solution; nevertheless, it does have several disadvantages. Opening the windows makes it challenging to control the indoor temperature. In places where there are high outdoor air pollution levels, it can also bring this into the building. Eventually, many offices have windows that cannot be opened.
2. Turn on HVAC & Central Air Systems
To address ventilation and COVID-19, If opening a window isn’t possible, then turning on the central air system or ‘HVAC’ could help enhance indoor ventilation. HVAC systems often take outdoor air and pump the air into all the areas in the building.
They also suck out air throughout vents, which could diminish the concentration of viruses in the area by sucking them outside.
HVAC systems, however, are complex. There are reports that HVAC systems have a role in spreading viruses such as the coronavirus. This occurs because they move airborne droplets from an infected person/area around the room or the building. On the other hand, ASHRAE explains that proper use of ventilation can reduce the airborne concentration of COVID-19 and thus the chance of transmission through the air.
HVAC systems that recirculate air should be fitted with air filters to diminish the chance of transmission of the virus.
HVAC systems can generally provide up to five air changes each hour, significantly improving indoor ventilation. Nonetheless, recirculation should be reduced/eliminated, and central air systems should be fitted with filters to evade the risk of further transmission.
3. Install a HEPA Filter
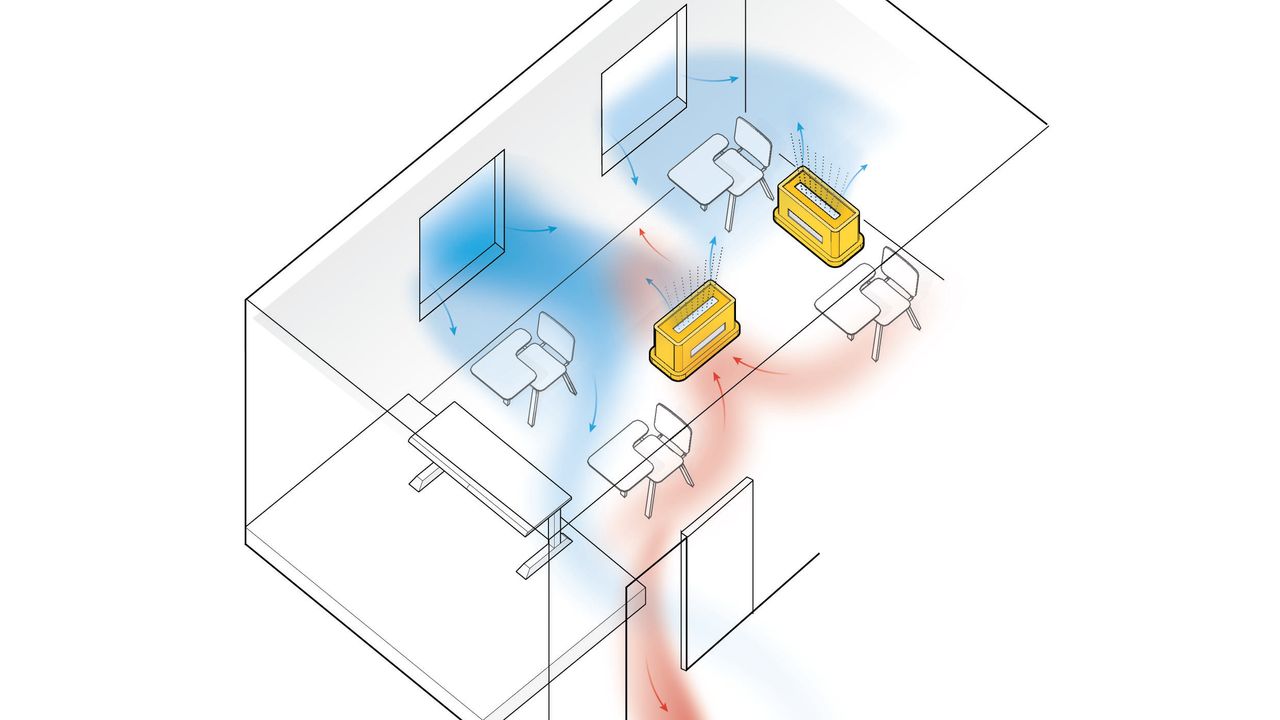
If there’s no central air system available, installing portable air purifiers is a third option to improve ventilation. Since air purifiers do not directly ventilate a room by replacing the inside air, they can do something like remove viruses from the air.
The calculation of how much air purifiers can increase ventilation is relatively simple. In the beginning, find the purifier’s airflow rate, either in m3/hr or cfm. Then calculate the room’s inside volume.
For example, the Smart Air Blast air purifier has an airflow of 1800 cbm/hr. The volume of a 100 sqm room with a ceiling height of 2.4 m is 240 m3. That means the Blast is able to provide: 1800/240 = 7.5 equivalent air changes per hour.
Air purifiers with HEPA filters are a simple solution to removing viruses from the air. The best part is that air purifiers don’t need to cost an arm and a leg. here are some notices about ventilation and COVID-19.
Notice #1: The position of the air purifier is especially vital in maximizing equivalent air changes per hour. If the purifier doesn’t improve the recirculation of the air in the entire room, its equivalent air changes per hour are likely to be much lower.
Notice #2: There are some concerns that viruses can survive on HEPA filters and be re-released into the air; however, data shows that the COVID-19 coronavirus and other enveloped viruses typically die in 72 hours on cardboard.
Key Messages about Ventilation and COVID-19
In the concept of ventilation and COVID-19, ventilation systems have alternatively been observed as a risky means of spreading COVID-19 or a straightforward technological fix to control the spread of the virus. Neither of these is firmly correct.
Although there is no evidence of HVAC systems dispersing the COVID-19 virus to distant occupants, HVAC systems are also inherently restricted in their ability to relieve the primary form of transmission (close range by large droplets). Nonetheless, HVAC systems play a significant role in healthy indoor air, and lack of ventilation almost certainly enlarges transmission risk. As such, the following should be thought for HVAC systems during the pandemic:
- Sharing spaces that do not contain ventilation systems with others increases the risk of COVID-19 transmission. Air conditioners and fans that recirculate room air should not be used without additional fresh air supply to the space. Air filtration may reduce the number of viruses in the air. Still, its effectiveness with respect to transmission reduction is unknown.
- Ensure that your ventilation system is operating well, regarding its design specifications. Verifying that your system is working suitably may require checking with an HVAC expert.
- Ventilation is a supporter, not a solution. Ventilation may lighten the risk of close-range aerosol transmission by preventing the accumulation of small particles in an enclosed space. However, most transmission is short-range droplets, which are unlikely to be affected or interrupted by most ventilation systems.
- Reduce crowding. Minimizing proximity to an infected person and duration of exposure are the most effective ways to reduce transmission.
- Follow infection control principles regularly. The fundamental infection control principles comprise: minimizing contact, hand hygiene, regular environmental cleaning, and disinfection, reducing crowding, using appropriate barriers (partitions, masks), protecting the susceptible, and prioritizing fresh air.
- If possible and safe, consider using natural ventilation, and opening windows.
- For mechanical systems, raise the outdoor air percentage, by means of economizer modes of HVAC. Before starting to increase outdoor air percentage, verify that your HVAC system is compatible with this change to control temperature and humidity. Furthermore, compatibility with outdoor/indoor air quality is of great importance.
- Increase total airflow supply to the working spaces, if possible.
- Disable demand-control ventilation controls that lower air supply based on occupancy or temperature.
- Enhance central air filtration:
- Increase air filtration to as high as achievable without significantly diminishing design airflow.
- Examine filter housing and racks to guarantee appropriate filter fit and check for ways to lessen filter bypass.
- Consider running the HVAC system at climax outside airflow for 2 hours before and after spaces are occupied, regarding the recommendation of the manufacturer.
- Generate clean-to-less-clean air movements by re-evaluating the positioning of supply and exhaust air diffusers and/or dampers and adjusting zone supply and exhaust flow rates to establish measurable pressure differentials. Have staff work in “clean” ventilation zones that do not include higher-risk areas such as visitor reception or exercise facilities (if open).
- Make sure exhaust fans in restroom facilities are functional and operating at full capacity when the building is occupied.
Buy Equipment or Ask for a Service
By using Linquip RFQ Service, you can expect to receive quotations from various suppliers across multiple industries and regions.
Click Here to Request a Quotation From Suppliers and Service Providers
Read More on Linquip
- Energy Recovery Ventilator (ERV): Installation, Types & Advantages
- Building Ventilation and Heat Dissipation: What You Need to Know
- Stack Ventilation: A Comprehensive Overview of The Principles and Applications
- The uprising of Digital Transformation in Covid-19 era
- HRV vs ERV: Choosing Between Remarkable Types of Ventilation Systems
- Heat Recovery Ventilation (HRV): Definition, Advantages & Installation
- Ventilation Design: Spectacular Tips You Need to Know
- HRV vs ERV: Choosing Between Remarkable Types of Ventilation Systems
- Natural Ventilation: Types, Advantages, and Disadvantages
- Home Ventilation: Necessity, Types, and Strategies
- Mechanical Ventilation System, Types, Advantages and Disadvantages
- 5 Types of Ventilation and All We Should Know About



Thanks for giving useful information in pandemic situation safety & precautions are most important for over health and safety
Dear Megri
Thanks for your Attention